
Hypogylcemia rescue (especially prehospital) If clinical response then start infusion of 2-5mg/h in 5% dextrose Beta-blocker or Calcium channel blocker toxicityĥmg IV bolus then repeat after 5min if no effect calcitonin by medullary carcinoma cells Pharmacological doses of glucagon also causes secretion of:
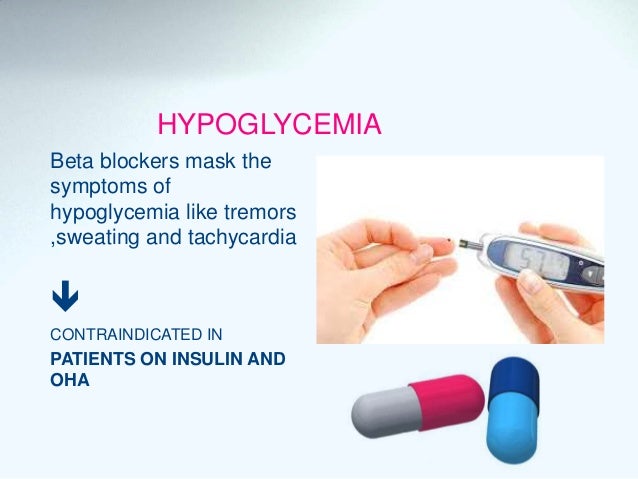
No effect on skeletal muscle (no glucagon receptors) LES): GI relaxation (may be caused by mechanisms independent of adenylyl cyclase) Liver and adipose tissue: glycogenolysis, gluconeogenesis, and ketogenesis resulting in increased blood CVS: positive inotropy and chronotropy similar to beta-agonists (but bypassing the adrenergic receptor) Agonist at glucagon-specific Gs-protein coupled receptor, activates adenylyl cyclase resulting in increased I Glucagon as an antidote for beta blocker or CCB toxicity evidence basis is often lacking and one therefore needs to rely on a combination of practical experience, case reports and assessment of biological plausibility. RATIONALE FOR GLUCAGON USE AS AN ANTIDOTE high-dose insulin as an antidote or supportive measures) risk of distraction from the delivery of other therapies (e.g. commonly induces vomiting, with concomitant aspiration risk in the unprotected airway In Australia, the toxicology community rarely advises the use of glucagon as an antidote, for these reasons: glucagon has also been used in the setting of calcium channel blocker toxicity Glucagon is traditionally considered a first line antidote for beta-blocker overdose The high cost and limited availability of glucagon may be the only factors precluding its future clinical acceptance. Glucagon-treated patients should be monitored for side effects of nausea, vomiting, hypokalemia, and hyperglycemia. The doses of glucagon required to reverse severe beta-blockade are 50 micrograms/kg iv loading dose, followed by aĬontinuous infusion of 1-15 mg/h, titrated to patient response. This suggests that glucagon's mechanism of action may bypass the beta-adrenergic receptor site.īecause it may bypass the beta-receptor site, glucagon can be considered as an alternative therapy for profound beta. These effects are unchanged by the presence of beta-receptor blocking drugs. Glucagon increases heart rate and myocardial contractility, and improves atrioventricular conduction. Medical complications of beta-blocker overdose include hypotension, bradycardia, heart failure, impaired atrioventricularĬonduction, bronchospasm and, occasionally, seizures.Ītropine and isoproterenol have been inconsistent in reversing the bradycardia and hypotension of beta-blocker overdose. The high cost and limited availability of glucagon may be the only factors precluding its future clinical acceptance.Glucagon therapy for beta blocker overdose The doses of glucagon required to reverse severe beta-blockade are 50 micrograms/kg iv loading dose, followed by a continuous infusion of 1-15 mg/h, titrated to patient response. Because it may bypass the beta-receptor site, glucagon can be considered as an alternative therapy for profound beta-blocker intoxications. This suggests that glucagon's mechanism of action may bypass the beta-adrenergic receptor site. Atropine and isoproterenol have been inconsistent in reversing the bradycardia and hypotension of beta-blocker overdose.
Medical complications of beta-blocker overdose include hypotension, bradycardia, heart failure, impaired atrioventricular conduction, bronchospasm and, occasionally, seizures. The effects of glucagon in reversing the cardiovascular depression of profound beta-blockade, including its mechanism of action, onset and duration of action, dosage and administration, cost and availability, and side effects are reviewed. Two cases of severe beta-blocker overdose are presented that were treated successfully with glucagon therapy.


 0 kommentar(er)
0 kommentar(er)
